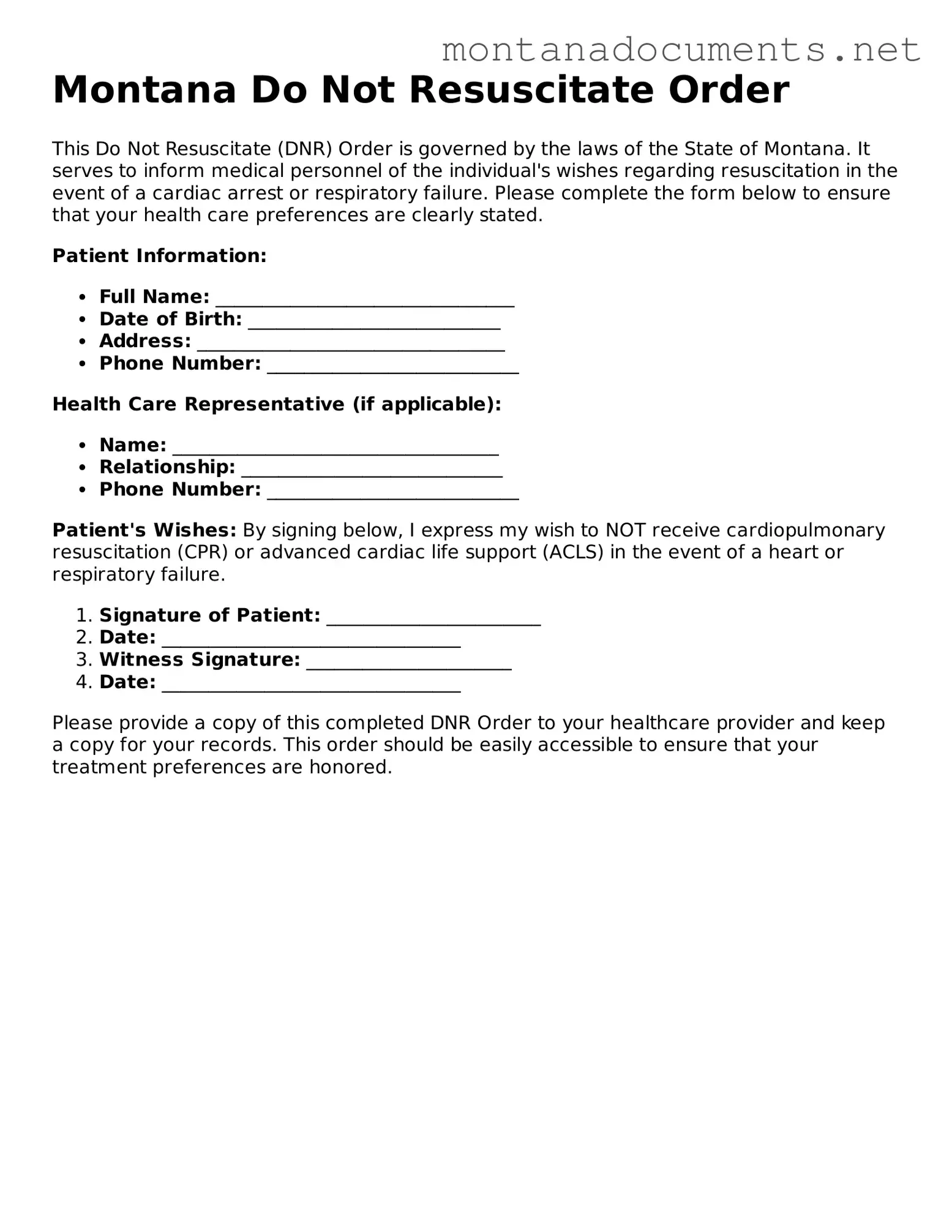
Blank Montana Do Not Resuscitate Order Document
Key takeaways
When considering a Do Not Resuscitate (DNR) Order in Montana, it is important to understand the following key points:
- Purpose of the DNR Order: This document communicates a person's wishes regarding resuscitation efforts in the event of cardiac or respiratory arrest.
- Eligibility: Individuals who are 18 years or older can complete a DNR Order. It is crucial that the person signing the form is capable of making informed decisions.
- Medical Provider's Role: A licensed healthcare provider must sign the DNR Order for it to be valid. This ensures that the order is based on medical advice and understanding of the individual's health condition.
- Distribution of the Order: Once completed, copies of the DNR Order should be provided to all healthcare providers involved in the individual's care, as well as family members.
- Revocation: The DNR Order can be revoked at any time by the individual or their legal representative. This can be done verbally or by destroying the document.
- Legal Protection: Healthcare providers are protected from legal liability when following a valid DNR Order, as long as they act in good faith.
- Review and Update: It is advisable to review the DNR Order periodically, especially if there are changes in health status or personal preferences regarding end-of-life care.
Similar forms
The Montana Do Not Resuscitate (DNR) Order form shares similarities with the Advance Directive, a legal document that outlines a person's wishes regarding medical treatment in the event they become unable to communicate. Both documents serve to ensure that an individual's preferences are respected during critical health situations. An Advance Directive can include a variety of instructions, such as preferences for life-sustaining treatments, and may also appoint a healthcare proxy to make decisions on behalf of the individual. This empowers individuals to have a say in their medical care, much like the DNR does specifically regarding resuscitation efforts.
Another document akin to the DNR Order is the Physician Orders for Life-Sustaining Treatment (POLST). This form is designed for patients with serious illnesses and translates their treatment preferences into actionable medical orders. Just as the DNR specifies a patient’s desire not to receive cardiopulmonary resuscitation (CPR), the POLST allows individuals to express their wishes regarding a broader range of life-sustaining treatments. Both documents require a healthcare professional’s signature, ensuring that the patient’s wishes are documented and respected by medical personnel.
The Living Will is another document that bears resemblance to the Montana DNR Order. A Living Will allows individuals to outline their preferences for medical care in situations where they may be incapacitated. While the DNR focuses specifically on resuscitation efforts, a Living Will can cover various aspects of end-of-life care, including preferences for pain management and other life-sustaining measures. Both documents aim to communicate the patient’s wishes clearly, thereby minimizing confusion for healthcare providers and family members during critical moments.
Similar to the DNR Order, the Medical Power of Attorney grants a designated person the authority to make medical decisions on behalf of someone else. This document comes into play when the individual is unable to express their wishes. While the DNR specifically addresses resuscitation, the Medical Power of Attorney encompasses a broader range of medical decisions. Both documents emphasize the importance of having a clear plan in place to ensure that healthcare decisions align with the individual's values and preferences.
The Healthcare Proxy is another document that parallels the DNR Order. It designates a trusted individual to make healthcare decisions on behalf of someone who is unable to do so. Like the DNR, which provides specific instructions regarding resuscitation, a Healthcare Proxy allows the appointed person to interpret the individual's wishes and make decisions in line with those preferences. Both documents serve to protect patient autonomy and ensure that care aligns with the individual’s desires.
In many legal proceedings, the submission of various forms is essential, including those that affirm the delivery of documents. A noteworthy example is the Affidavit of Service form, which verifies the proper serving of legal papers, an integral step in the judicial process. Just as other documents delineate preferences in healthcare decisions, the Affidavit of Service encapsulates a critical declaration that supports the integrity and progression of legal actions.
The Comfort Care Order, while not as widely recognized, shares similarities with the DNR Order in that it focuses on the quality of life rather than aggressive medical interventions. This document outlines the desire for comfort measures only, without the use of life-sustaining treatments. Like the DNR, it emphasizes the importance of patient comfort and dignity in end-of-life care, ensuring that healthcare providers understand the individual’s priorities during critical health situations.
The Do Not Intubate (DNI) Order is another document that is closely related to the DNR Order. A DNI specifies that a patient does not wish to be placed on a ventilator if they are unable to breathe on their own. While the DNR addresses resuscitation efforts more broadly, the DNI focuses specifically on the use of mechanical ventilation. Both documents reflect the patient’s wishes regarding interventions that may prolong life but do not necessarily improve its quality.
The End-of-Life Care Plan can also be likened to the DNR Order. This comprehensive document outlines an individual’s preferences for all aspects of care at the end of life, including pain management, resuscitation, and emotional support. While the DNR focuses solely on resuscitation, the End-of-Life Care Plan provides a more holistic view of the individual's desires, ensuring that all aspects of their care align with their values and wishes.
Finally, the Hospice Care Plan shares similarities with the DNR Order in that both documents prioritize comfort and quality of life for patients with terminal conditions. The Hospice Care Plan outlines specific goals for care, focusing on symptom management and emotional support rather than curative treatments. In this way, both documents reflect a shift in focus from aggressive medical interventions to a more compassionate approach to end-of-life care.
Consider More Forms for Montana
What Is a Poa Document - A General Power of Attorney allows an individual to designate another person to act on their behalf in legal matters.
Obtaining accurate information can be crucial, and that’s where an Employment Verification Form comes into play, offering essential details concerning an individual’s job history. For those in need of a reliable template for such forms, resources like TopTemplates.info can be incredibly helpful.
Montana Medical Power of Attorney - With this form, you can hand-pick a healthcare decision-maker who understands your values and preferences.
Common mistakes
-
Incomplete Information: Many individuals fail to provide all required personal details, such as the patient's name, date of birth, and signature. Omitting this information can lead to confusion and may invalidate the order.
-
Incorrect Witness Signatures: Some people overlook the need for proper witness signatures. The form typically requires two witnesses who are not related to the patient or beneficiaries. Ignoring this requirement can render the document ineffective.
-
Not Understanding the Implications: A common mistake is not fully grasping what a Do Not Resuscitate (DNR) order entails. This can lead to misunderstandings about the level of care the patient will receive in an emergency.
-
Failure to Communicate: Individuals often forget to discuss their wishes with family members and healthcare providers. Without open communication, there may be confusion or disagreement about the patient's preferences during a medical emergency.
-
Using Outdated Forms: Some people mistakenly use older versions of the DNR form. It is crucial to ensure that the most current version is utilized, as regulations may have changed.
-
Not Reviewing the Form Regularly: Individuals may fill out the form but neglect to review it periodically. Changes in health status or personal wishes should prompt a review and possible update of the DNR order.
Documents used along the form
In Montana, the Do Not Resuscitate (DNR) Order form is an important document for individuals who wish to communicate their preferences regarding resuscitation in medical emergencies. However, it is often accompanied by other forms and documents that support a person's healthcare decisions. Below is a list of these documents, each serving a unique purpose in the realm of medical care and decision-making.
- Advance Directive: This document outlines a person's wishes regarding medical treatment and end-of-life care. It can specify preferences for life-sustaining treatments and appoint a healthcare proxy.
- Healthcare Power of Attorney: This legal document designates someone to make medical decisions on behalf of an individual if they become unable to do so themselves.
- Living Will: A living will expresses an individual's wishes about medical treatment in situations where they are unable to communicate their desires, particularly regarding life support.
- Physician Orders for Life-Sustaining Treatment (POLST): This form translates a patient's treatment preferences into actionable medical orders, ensuring that healthcare providers honor those wishes.
- Patient Information Form: This form collects essential information about the patient, including medical history, allergies, and current medications, to assist healthcare providers in delivering appropriate care.
- Medical Release Form: This document allows healthcare providers to share a patient's medical information with designated individuals, facilitating communication among family members and caregivers.
- ATV Bill of Sale Form: To facilitate the transfer of ownership for all-terrain vehicles, refer to our comprehensive ATV Bill of Sale resources that ensure all legal requirements are met.
- Organ Donation Registration: This form indicates a person's wishes regarding organ donation after death, ensuring that their preferences are respected.
- Do Not Hospitalize Order: This order specifies that a patient should not be admitted to a hospital, often used for individuals in long-term care settings who wish to avoid hospitalization.
- Medication Administration Record: This record tracks medications administered to a patient, ensuring that their treatment plan is followed accurately.
Each of these documents plays a critical role in ensuring that healthcare providers understand and respect an individual's wishes regarding medical care. By having these forms in place, individuals can feel more secure in knowing their preferences will be honored during critical moments.
Misconceptions
Understanding the Montana Do Not Resuscitate (DNR) Order form is crucial for individuals making end-of-life decisions. However, several misconceptions can cloud judgment. Here are eight common misunderstandings:
- A DNR means no medical care at all. Many believe that signing a DNR means refusing all medical treatment. In reality, a DNR specifically addresses resuscitation efforts during cardiac or respiratory arrest, while other medical treatments can still be provided.
- Only terminally ill patients can have a DNR. This is not true. Anyone can request a DNR, regardless of their health status. It’s a personal choice that reflects individual values and preferences.
- A DNR is only valid in hospitals. Some think that a DNR is only applicable in hospital settings. However, a valid DNR order is recognized in various healthcare environments, including at home and in long-term care facilities.
- Signing a DNR means giving up hope. Many people associate a DNR with a loss of hope. In fact, it can represent a thoughtful decision to focus on quality of life rather than aggressive interventions.
- Family members can override a DNR. While family discussions are important, a legally signed DNR cannot be overridden by family members once it is in place. Healthcare providers must follow the documented wishes of the patient.
- A DNR is permanent and cannot be changed. This misconception leads to concern about being locked into a decision. In reality, a DNR can be revoked or modified at any time by the patient or their legal representative.
- All DNR orders are the same. People often assume that all DNR forms have the same legal weight. However, DNR orders can vary by state and must comply with local laws to be valid.
- Healthcare providers will not respect a DNR. There is a fear that medical professionals may ignore a DNR order. In fact, healthcare providers are legally obligated to honor a valid DNR and respect the patient’s wishes regarding resuscitation.
By dispelling these misconceptions, individuals can make informed choices about their healthcare preferences and ensure their wishes are respected in critical situations.
Understanding Montana Do Not Resuscitate Order
-
What is a Do Not Resuscitate (DNR) Order?
A Do Not Resuscitate Order is a legal document that allows individuals to refuse certain medical interventions, specifically cardiopulmonary resuscitation (CPR), in the event of cardiac arrest or respiratory failure. In Montana, this order must be completed and signed by a physician and the patient or their legal representative.
-
Who can request a DNR Order in Montana?
Any adult who is capable of making their own medical decisions can request a DNR Order. Additionally, a legal representative can request this order on behalf of a patient who is unable to make decisions due to incapacity.
-
How do I obtain a DNR Order form in Montana?
You can obtain a DNR Order form from your healthcare provider, hospital, or through the Montana Department of Public Health and Human Services. It's important to ensure that the form is completed correctly to be valid.
-
What information is required on the DNR Order form?
The DNR Order form typically requires the following information:
- The patient's name and date of birth
- The name of the physician completing the order
- Signatures of both the patient (or their legal representative) and the physician
- The date the order was signed
-
Is a DNR Order valid in all healthcare settings?
Yes, once properly completed and signed, a DNR Order is valid in all healthcare settings, including hospitals, nursing homes, and at home. However, it's crucial to ensure that the order is readily available and communicated to all healthcare providers involved in the patient’s care.
-
Can a DNR Order be revoked?
Yes, a DNR Order can be revoked at any time. The patient or their legal representative should communicate their decision to revoke the order to their healthcare provider and ensure that the order is removed from their medical records.
-
What happens if a DNR Order is not followed?
If a DNR Order is not followed, it can lead to unnecessary medical interventions that the patient did not want. This may result in distress for the patient and their family. Healthcare providers are legally obligated to respect valid DNR Orders.
-
How does a DNR Order affect other medical treatments?
A DNR Order specifically addresses resuscitation efforts and does not affect other medical treatments. Patients can still receive comfort care and other interventions, such as pain management and medications, as desired.